Submitted by Washington State Department of Health
It is tough to think about how to address pressing social problems like institutional racism and oppression when we are already dealing with a pandemic. Some of us make decisions to protest in large groups by weighing the risk of catching and spreading COVID-19 to our family against the urgent need to change the way we think about race in this country.
It’s a lot at once, and we haven’t even really started with the “murder hornets” yet.
Pandemics don’t come when they are convenient. In March 1918, when the first cases of pandemic flu were identified, we were fighting World War I. So, they were busy back then too.
During the 1918 flu pandemic, about 500 million people — about a third of the world’s population at the time — got flu. 50 million people died from it. There was no vaccine. There were no good treatments — either for the flu or for the bacterial pneumonia that sometimes followed. The health care systems around the country were totally overwhelmed, and people couldn’t get the care they needed.
There are big differences between that pandemic and this one. For starters, the 1918 flu pandemic was caused by an influenza virus, and COVID-19 is caused by a coronavirus. And the world was a different place then, with much slower travel options, fewer people, but in a lot of places, more crowding.
Still, the 1918 flu pandemic taught us important lessons that resonate still today. Here are three:
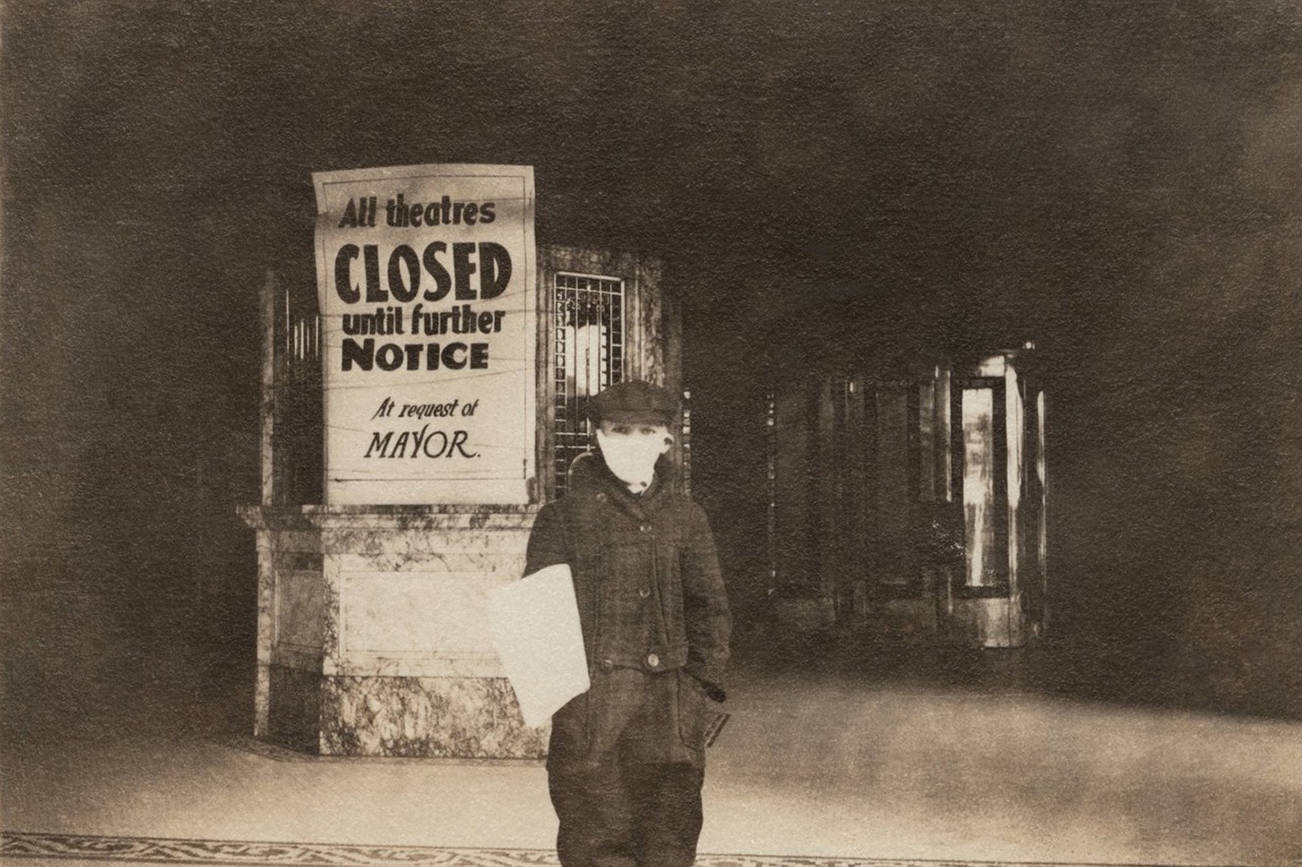
1. Trusted tools work. In 1918, there was no World Health Organization, and there was no US Centers for Disease Control and Prevention. Each city responded to the pandemic on their own. Cities took action by counting the number of people who got flu, by isolating and quarantining families who were sick, by closing theaters and public transportation, by requiring masks in public. Sound familiar? When cities were able to consistently implement these tools, they flattened the curve. When they strayed from these approaches, more people got sick.
2. Pandemics aren’t fair. Today, COVID-19 highlights differences in health and health care experiences among people with different types of privilege. Similarly, in 1918, people were not all impacted equally. People who had underlying health conditions were more likely to die. Soldiers and people who lived in poverty and crowded conditions were more likely to get sick. Pandemics happen in diverse communities. To stop the spread, everyone in the community needs the opportunity to be healthy.
3. We cannot do this alone. We value our independence, but pandemics teach us how interdependent we really are. We’re not the only ones with influence on our health. It matters for your health whether I wear a mask. Your health is impacted if I decide to go out in public with a bit of a cough. You may need hospital care, but if we all haven’t done our part to stop the spread of COVID-19, there may be no room for you. If my employer doesn’t provide affordable health insurance, I may not be able to get the preventive care I need. The 1918 flu highlighted how connected we all are. After the pandemic, many nations responded by providing guaranteed health care to all their residents. The flu, like COVID-19, respected no county, state, or national border. In 1919 The International Bureau for Fighting Epidemics, a forerunner of WHO, was formed.
Some historians have observed that over time, we stopped talking about the 1918 pandemic, and some of these lessons were forgotten. But, they are important lessons, and we are learning them again. This time, let’s make sure we remember.
Practice compassion. We are all connected. Wash your hands, wear your cloth face covering, and stay home if you are sick. This is how we take care of each other.